Artificial Intelligence in Periodontal Diagnosis: Are Algorithms Ready to Sit Chairside?
Can a Machine See Gum Disease Better Than We Can?
Periodontitis is not subtle. Bone loss, inflamed gingiva, deep pockets—these are findings every clinician is trained to recognize. And yet, despite decades of refinement in periodontal indices and classification systems, diagnosis remains surprisingly variable. Why do two experienced clinicians sometimes stage the same patient differently?
Now imagine this question: What if a machine could see periodontal destruction with more consistency than the human eye—and do it in seconds?
This is no longer science fiction. According to a 2025 narrative review by Shaker et al., artificial intelligence (AI), particularly deep learning models such as convolutional neural networks (CNNs), is rapidly reshaping how periodontal diagnosis may be performed in the near future .
But how strong is the evidence—and how close are we to real clinical integration?
Why Periodontal Diagnosis Needs Help
Periodontitis is a multifactorial chronic inflammatory disease that affects up to 10–15% of adults worldwide and as many as 70% of adults in certain regions, including Egypt. Its impact extends beyond tooth loss, contributing to systemic conditions such as type 2 diabetes and cardiovascular disease.
Despite this burden, diagnosis still depends on:
- Manual probing depth measurements
- Clinical attachment loss (CAL)
- Bleeding on probing (BOP)
- Radiographic interpretation of bone loss
Each of these is operator-dependent, time-consuming, and prone to inter-examiner variability.
Even with the introduction of the 2017 AAP/EFP staging and grading system, clinicians must synthesize multiple data streams—radiographs, systemic risk factors, historical progression—often under real-world time constraints. This is precisely where AI enters the conversation.
What Exactly Is AI Doing in Periodontology?
Artificial intelligence, as described in the review, refers primarily to machine learning (ML) and deep learning (DL)systems trained on large datasets to recognize patterns that correlate with disease.
Among these, convolutional neural networks (CNNs) dominate periodontal research due to their effectiveness in image analysis.
In simple terms:
- CNNs break images into layers of features
- They learn what “bone loss,” “furcation involvement,” or “healthy crestal bone” looks like
- With sufficient training, they can classify disease severity with remarkable accuracy
Unlike traditional rule-based software, these systems learn from data—improving performance as datasets expand.
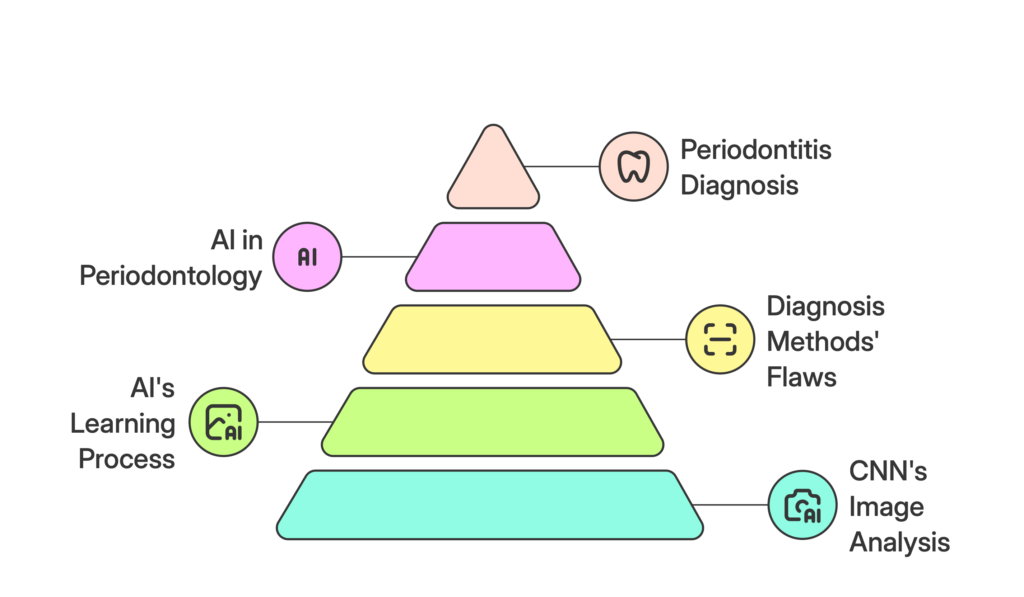
Radiographs: Where AI Performs Best
One of the strongest bodies of evidence lies in radiographic interpretation.
Several studies summarized in the review demonstrate that CNNs can detect alveolar bone loss on periapical, bitewing, and panoramic radiographs with diagnostic accuracy comparable to or exceeding experienced clinicians.
Key findings include:
- CNNs achieving AUC values around 0.92 for bone loss detection
- Automated measurement of bone loss percentages
- Consistent performance across thousands of images
More advanced systems now integrate cone-beam computed tomography (CBCT), enabling 3D assessment of periodontal destruction. One notable system, PerioAI, achieved an accuracy of 94.4% and sensitivity of 100%, outperforming expert periodontists in controlled settings.
This suggests a future where radiographs are not merely viewed, but interpreted algorithmically in real time.
Beyond Bone: AI and Clinical Periodontal Parameters
Radiographs tell only part of the story. Periodontal diagnosis also depends on soft-tissue findings—gingival inflammation, plaque accumulation, recession, and bleeding.
Recent AI models have begun analyzing:
- Intraoral photographs
- 3D intraoral scans
- Color and texture changes of gingival tissues
CNNs trained on annotated clinical images can now:
- Identify gingival margins
- Detect plaque and calculus
- Estimate gingival inflammation with AUC values exceeding 0.90
These systems promise something clinicians have long struggled with: objective digital periodontal charting. Instead of manually recording subjective indices, AI could generate standardized, reproducible measurements—useful for both diagnosis and patient motivation.
Can AI Stage and Grade Periodontitis?
Perhaps the most clinically exciting development is AI’s ability to align with the 2017 classification system.
Several deep learning models now:
- Automatically estimate radiographic bone loss
- Assign periodontal stage (I–IV)
- Predict grade (A–C) by incorporating systemic risk factors
Hybrid models—combining CNNs with algorithms like random forests or support vector machines—integrate:
- Smoking status
- Diabetes
- Age
- Clinical measurements
In some studies, automated staging and grading achieved accuracies exceeding 95%, matching expert consensus. This raises a provocative question:
If AI can consistently apply complex classification criteria, should clinicians continue doing this manually?
The Promise: Why AI Could Transform Periodontal Care
If implemented responsibly, AI offers several compelling advantages:
- StandardizationReduced inter- and intra-examiner variability
- EfficiencyFaster diagnosis and documentation
- Decision SupportReal-time risk prediction and treatment planning
- Longitudinal MonitoringObjective tracking of disease progression
- AccessibilityPotential support in low-resource or underserved settings
Rather than replacing clinicians, AI functions as a clinical co-pilot, augmenting human judgment with data-driven consistency.
The Reality Check: Why AI Is Not Chairside—Yet
Despite impressive performance metrics, the review is clear: most AI systems remain experimental.
Key limitations include:
- Small, single-center datasets
- Limited demographic diversity
- Annotation bias from expert labeling
- Lack of prospective clinical trials
- “Black-box” model behavior
Regulatory hurdles are significant. For FDA or equivalent approval, AI systems must demonstrate:
- Transparency (explainable AI)
- Reproducibility
- Safety across populations
- Seamless integration into clinical workflows
At present, many models perform brilliantly in controlled environments—but struggle with real-world variability.
Ethical and Practical Considerations
Beyond performance, AI introduces ethical questions:
- Who is responsible for diagnostic errors?
- How is patient data protected?
- Can clinicians trust recommendations they cannot explain?
The review emphasizes the need for:
- Ethical frameworks
- Clear accountability
- Patient consent and data governance
Without these safeguards, even the most accurate algorithms will face resistance.
Conclusion: So—Is AI Ready for Periodontology?
Not quite. But it’s closer than many realize.
Artificial intelligence has already demonstrated the ability to:
- Detect periodontal bone loss with high accuracy
- Quantify clinical parameters objectively
- Automate staging, grading, and risk prediction
The next phase is not technological—it is clinical validation, explainability, and integration.
If researchers, clinicians, and regulators collaborate effectively, AI-assisted periodontal diagnosis could move from research papers to routine care within the next decade.
The real question may no longer be whether AI belongs in periodontology—but how thoughtfully we choose to adopt it.
Key Takeaway
“Artificial intelligence won’t replace periodontists—but it may redefine what diagnostic consistency looks like.”
Reference
Shaker, N., Ezzatt, O. M., Abbas, W., & Abdalwahab, M. M. (2025). Artificial intelligence in periodontal diagnosis: Current evidence and future clinical integration. International Journal of Chemical and Biochemical Sciences, 27(22), 16–23. https://doi.org/10.62877/2-IJCBS-25-27-22-2

Leave a Reply